
Juan Sanchez-Ramos, MD, PhD, has dedicated much of his career to learning everything
he can about Huntington’s disease, a rare hereditary neurodegenerative illness that
impacts cognition, mood and movement.
His work has filled the medical literature with findings that offer a better understanding
of how the disease begins, progresses, and is passed on to progeny. His work has led
to a more practical method for delivery of gene therapy via a nose-to-brain instillation
of nanoparticles. This approach is safe, non-invasive and does not need neurosurgical
intervention.
This month, Dr. Sanchez-Ramos is retiring from USF Health, leaving a legacy of valuable
work and a story for others to know – that the path into and across a career is not
always a straight line.
He has been with USF Health since 1996.
Dr. Sanchez-Ramos is the Helen Ellis Professor of Neurology and director of the HDSA
Huntington’s Disease Center of Excellence in the USF Health Morsani College of Medicine.
He is a prominent figure in neurodegenerative disease research and patient care, especially
in Huntington’s disease, an inherited brain disorder that leads to a gradual decline
in movement, mood, and cognitive functions.
The USF Health Huntington’s Disease Center of Excellence, established in 2006 and
supportd by the HD Society of America, has been instrumental in advancing gene therapies
for Huntington’s disease and has been a transformative resource for its patient’s
lives.

The USF Health Huntington’s Disease Center of Excellence & USF Health Byrd Alzheimer’s Center and Research Institute.
At the start of Dr. Sanchez-Ramos's career, he was Initially drawn to medicine by
his father’s influence. However, he found himself equally captivated by the world
of art during his undergraduate years at the University of Chicago while studying
pre-medicine. After receiving his bachelor's degree, Dr. Sanchez-Ramos made a bold
decision – to drop out of school and pursue a career as an artist.
He embarked on a 3 year artistic journey in Paris, where he initially planned to study
at the Ecole des Beaux Arts. He never did enroll in the Academy and worked as a free-lance
artist in Paris, Malaga and Copenhagen. He finally realized the life of an artist
is very difficult, and he redirected his career to the study of Neurosciences and
Medicine. While attending graduate school at the university, he pursued graduate
studies in neuropharmacology and ended up doing his PhD on the mechanisms of opioid
tolerance, dependence, and withdrawal.
A paper came out that uncovered an opioid analog made in an underground lab was producing
symptoms of Parkinson’s through IV opioid abuse. This sparked Dr. Sanchez-Ramos's
interest because it provided a link between his basic research on opioids and its
potential cause of neurological diseases like Parkinson's. This inspired him to go
to medical school at the University of Illinois in Chicago. In this transition from
his basic research to medical school, he followed up with a neurology residency and
a fellowship in movement disorders.
Decades later he was invited by Nancy Wexler, a renowned geneticist, to be involved
in the Huntington’s Disease Research project. The research gathered led to a significant
breakthrough — the discovery in 1992 of the Huntington’s disease gene.
Soon after, Dr. Sanchez-Ramos was recruited to the USF, where he would establish a
cutting-edge lab and clinic and hold the Helen Ellis Endowed Chair. Initially, it
was focused on Parkinson’s disease but later it expanded to Huntington’s Disease.
Through multidisciplinary collaboration, Huntington’s Disease Center of Excellence
at USF Health provides comprehensive care for patients, recognizing the complex array
of symptoms that accompany these devastating neurological disorders. By 2006, it had
annual grants from the Huntington's Disease Society of America in New York to operate
as a center of excellence.
“This was an incredible blessing to all these patients and their families to have
this in place... But in addition to that, it has created a cohort of patients that
we have been able to follow, study, and test new gene therapy treatments of Huntington’s
disease that have the potential to treat or cure the disease.” Dr. Clifton Gooch MD,
professor and chair of the USF Health Morsani College of Medicine’s Department of
Neurology,
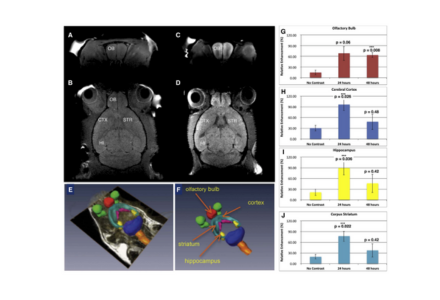
Image showing nanoparticle delivery system findings.
While at USF Health, Dr. Sanchez-Ramos and his team developed a nanoparticle system
that could be loaded with gene modifying molecules and could be delivered intranasally
to combat the progression of Huntington’s disease. This was partially funded by the
National Institute of Neurological Disorders and Stroke in the NIH. Dr. Sanchez-Ramos
and colleagues continue to seek funding to pursue this gene therapy treatment even
further.
“The goal is to prevent this from happening,” Dr. Sanchez-Ramos said. “We already
can identify those individuals who carry the genetic mutation. We know the earlier
that we can start treatment the less likely the person will develop the illness. So,
if we identify a person who has the mutated gene and we can give therapy that prevents
the expression of the mutant gene, that would a great accomplishment, in essence,
a cure for Huntington’s disease.”
“He's the one who completely set this up from the very beginning,” Dr. Gooch said.
“The clinic has helped hundreds of families and patients. In addition to playing a
role in helping push this work forward... I think the work that Juan and others have
done is going to lead us to a cure for Huntington’s disease.”
Photos, video, and story by Ryan Rossy, USF Health Communications