The symptoms can’t be ignored: You’re losing concentration and sleep; have little appetite, motivation or energy; and almost no self-esteem. Worse, suicidal thoughts creep into your head.
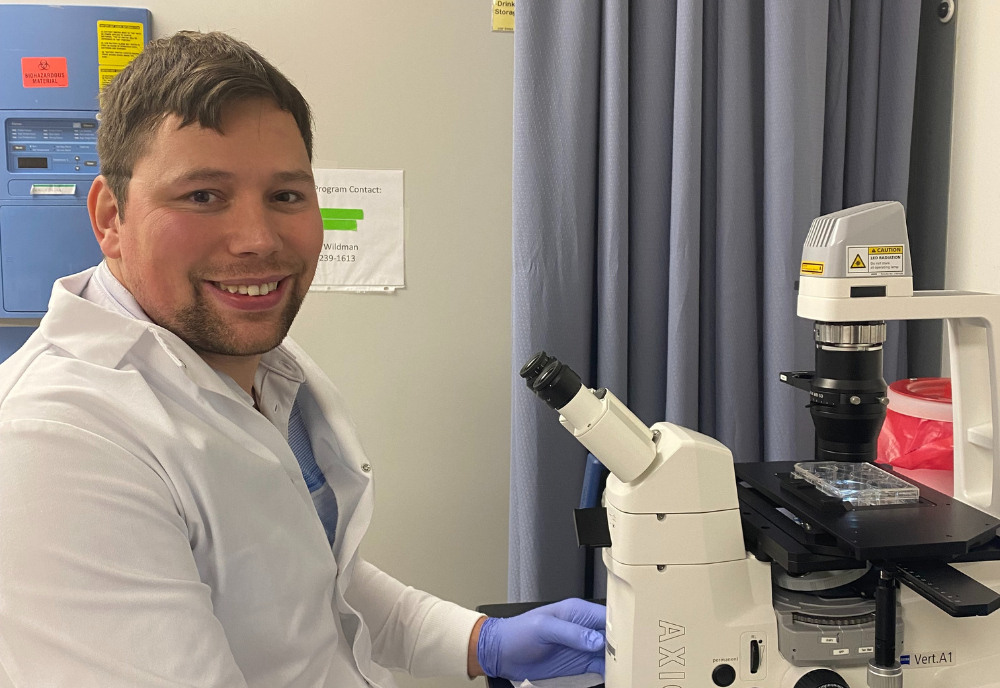
Jan Dahrendorff, a College of Public Health (COPH) PhD student in USF’s Genomics Program wants to change that scenario. In a paper published in the American Journal of Medical Genetics, Dahrendorff has added to the extensive literature on what is known as major depressive disorder, or MDD.
“It’s one of the leading causes of disability in the United States and globally and a serious socio-economical health problem that needs more attention,’’ Dahrendorff said. “MDD brings a range of negative consequence short and long-term: missed life opportunities, an economic impact of over $326 billion in the United States alone and in the most extreme cases it can lead to suicide.’’
Dahrendorff explains the results of his research in the journal report titled, “Leveraging DNA methylation to predict treatment response in major depressive disorder: A critical review.”
Research for the paper involved epigenetics, the study of how a person's environment and behaviors can affect their genes, but without changing their DNA sequence. Dahrendorff put this in the context of psychiatric disorders. He then looked at differences in DNA methylation, a chemical process that regulates gene expression by turning genes on or off without altering the underlying DNA sequence.
(Photo courtesy of Dahrendorff)
“The investigation of DNA methylation in the context of depression treatment outcomes is an emerging field and we wanted to summarize existing studies, and to inform our own research,’’ he said. “The majority of such studies are antidepressant treatments and only a few focus on brain stimulation treatments or psychotherapy.’’
The findings of his research, he said, “highlight the need for reliable predictors of MDD treatment outcomes, biological or social factors that could inform which patients might benefit from a certain treatment.’’
Ultimately, Dahrendorff hopes his work will help bring medical science closer to better therapies for people suffering from MDD.
“The research paper highlights the currently unmet need of predictors of treatment outcomes,’’ he said. “I hope that research into epigenetic characteristics between responders and non-responders of depression treatments can lead to more effective care in depression.’’

(Photo courtesy of Dahrendorff)
As lead author of the paper, Dahrendorff worked with two USF colleagues who co-authored the journal paper: Dr. Glenn Currier, former chair of the department of psychiatry at the Morsani College of Medicine, Dr. Monica Uddin, a professor in the USF Genomics Program.
“Jan’s work is based on a paper he originally drafted in one of his PhD classes and he’s developed it into a published work,’’ Uddin said. “More importantly, he has used this work to set the stage for several empirical studies for his PhD.’’
Dahrendorff also is working on a study that has not yet been published. It involves blood samples of patients with MDD before, during and after transcranial magnetic stimulation treatment − a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. The goal is to characterize epigenetic differences among treatment responders and non-responders. The majority of the study participants took a variety of antidepressants, but with no success.
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest, according to the Mayo Clinic, the world’s largest integrated, not-for-profit medical group practice. Also called clinical depression, it affects how someone feels, thinks and behaves and can lead to a variety of emotional and physical problems.
For more information about MDD, visit https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007